Doctors Suffering Burnout Need Compassion Not Blame, Says Top GP
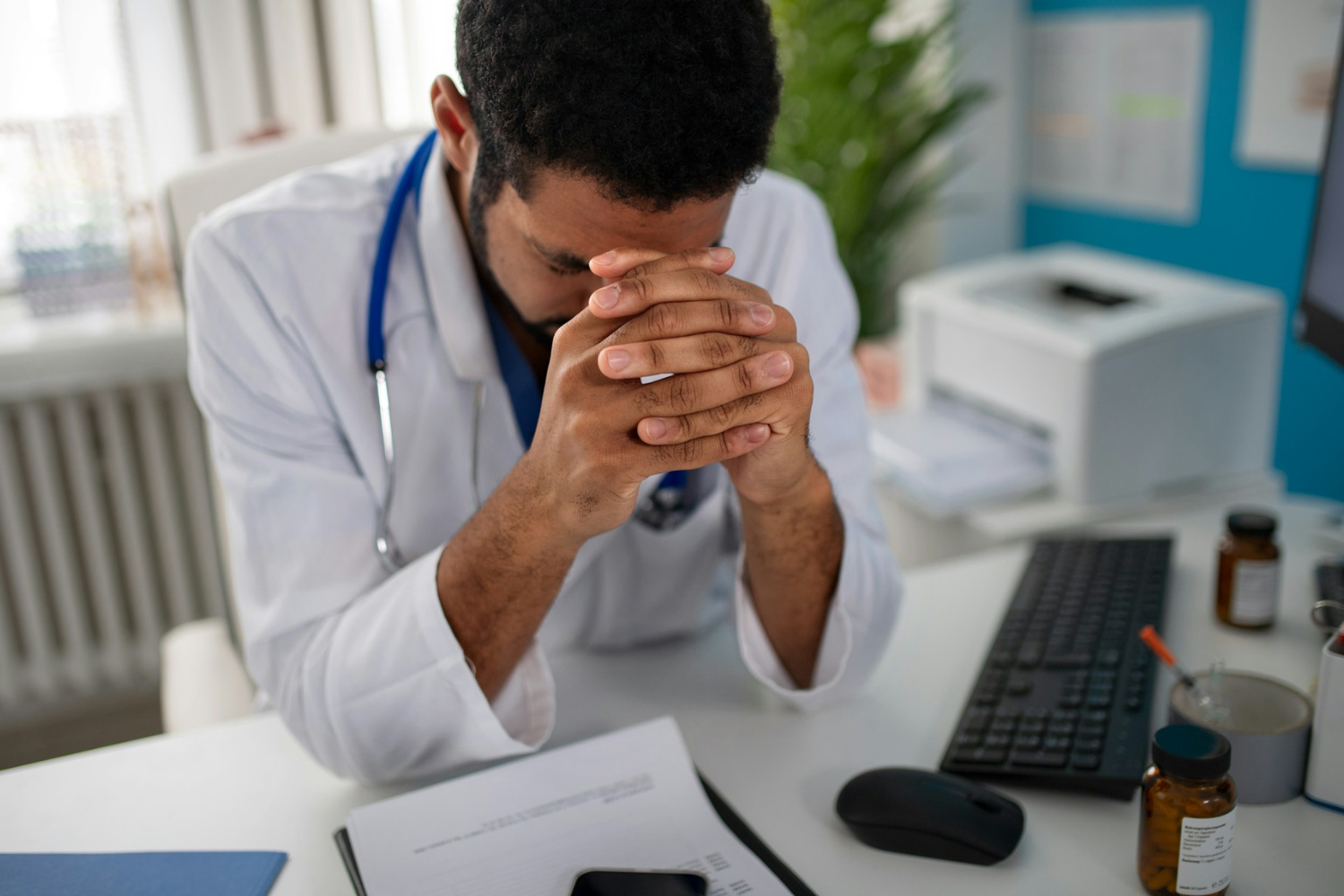
Image by Getty Images for Unsplash+
Doctors, nurses and other healthcare staff suffering burnout should be shown compassion and not blamed for being unwell, according to a leading GP.
Clare Gerada says employers often treat physicians as ‘naughty schoolchildren’ when they go sick or suffer mental health problems. Professor Dame Gerada, past president of the Royal College of General Practitioners (RCGP), is calling for more comprehensive guidance that focuses on ‘kindness’ and ‘sensitivity’.
The doctor, who helped found mental health charity Doctors in Distress, addresses the need for major reform in a new book aimed at reforming care for doctors and nurses with mental illness.
The Handbook of Physician Mental Health, publishing next week, highlights how suicide rates for doctors are up to four times those of other professional groups. GPs, psychiatrists and doctors trained overseas are among the healthcare workers who are especially at risk.
So are female clinicians who face the burden of a ‘second shift’ – caring for patients during the day and their families at night.
A global workforce crisis fuelled by increased workload and bullying and racism are among numerous factors identified in the book for clinicians developing depression, anxiety and other mental health problems.
Another key risk factor is what Professor Gerada describes ‘the industrialisation of care’ where too much focus is placed on meeting strict targets at the expense of providing personalised healthcare for patients.
The Handbook of Physician Mental Health references high-profile cases where doctors have died by suicide including junior doctor Rose Polge in 2016 and psychiatrist Daksha Emson who took her life and that of her daughter in 2000.
Professor Gerada says: “General practice across the world is in crisis. Workload has increased substantially in recent years and has yet to be matched by growth in either funding or workforce.
“Fear is at the heart of the factors contributing to physician mental illness and suicide. Doctors fear losing their professional identity, being cast out of medicine, becoming a patient, being abused and excluded, making mistakes, upsetting seniors and failing to meet patient expectations.
“Sick health professionals want to be treated compassionately – with sensitivity, sympathy, empathy and non-judgmentally. However, trainers, employers and regulators often treat them as naughty schoolchildren or wrongdoers for crossing the boundary from practitioner to patient.
“Many in authority over doctors wrongly conflate illness with a performance issue, like a disciplinary issue that needs to be addressed.”
This evidence-based handbook provides comprehensive insights into why doctors become unwell, how to identify those at risk, and the best approach to aid their recovery. It draws on learning from NHS Practitioner Health, a mental health which supports around 6,500 health and care professionals a year.
Among patient case histories featured in the book is a first-hand account by Sarinda Wijetunge, a junior doctor who was admitted to a mental health unit. Dr Wijetunge says doctors are ‘pushed to their limits by the job’s demands’.
The General Medical Council and British Medical Association does provide guidance on how doctors should behave when unwell or consulting with a sick colleague. But Professor Gerada says the advice is couched in ‘the language of blame, harm and avoiding problems – not focused on compassion’.
Patient complaints are a significant factor in suicide among doctors who derive self-worth from their jobs. The book explains that allegations of wrongdoing or unsatisfactory treatment can challenge the self-perception of healthcare workers as unsocial hours, working night shifts and moving frequently for career progression put doctors at risk of loneliness and increases their odds of developing mental health issues. The author says: “Doctors can find themselves surrounded by people and yet very much alone.”
Professor Gerada also outlines the barriers that exist to healthcare workers getting the help they need. Fear of losing confidentiality, a belief among the public that doctors are immune to illness, and their training which requires them to place patient need above place their patient’s needs above their own are among the reasons why they may hide their illness.